Hemoglobin C disorders are one of the most common structural hemoglobin variants. Hemoglobin C occurs due to a substitution of lysine for glutamic acid (glutamate) in position 6 of the beta-globin gene (leading to an abnormal hemoglobin A). Hemoglobin C is inherited in an autosomal recessive fashion. The gene has the highest frequency among individuals of African heritage although it is also present in Middle Eastern and Mediterranean descent including Turkey, Italy, and Greece. Therefore, patients with hemoglobin C can have one or two affected beta-globin chains leading to various degrees of severity of the disorder. Most individuals with hemoglobin CA (heterozygous state) are generally asymptomatic while those with hemoglobin CC can have chronic hemolytic anemia and other complications. Furthermore, hemoglobin C disorders can combine with other hemoglobin variants such as hemoglobin S leading to sickle cell disease (hemoglobin SC disease).
Epidemiology of Hemoglobin C
- Hemoglobin C is carried in up to 30% of individuals in Africa, particularly in West African countries such as Ghana, Burkina Faso, and Mali.
- Can also be found in the Middle East, Mediterranean, and other countries throughout the world, particularly in the heterozygous (carrier state).
Pathogenesis of Hemoglobin C
- Abnormality in normal hemoglobin A due to a beta-globin gene substitution of lysine for glutamate in position 6.
Most Common Hemoglobin C Patterns
There are four commonly found patterns of hemoglobin C:
- Hemoglobin C Trait: Heterozygous state (one out of two beta-globin genes affected). Most individuals do not develop any symptoms but a low mean corpuscular volume (MCV) and target cells could be found.
- Hemoglobin C Disease: Homozygous state (both beta globin genes affected). In general, it manifests with mild to moderate hemolytic anemia that can be identified in the first months of life. Individuals may develop splenomegaly and clinical features of anemia and hemolysis (jaundice, gallstones, etc.). Rarely, patients could develop musculoskeletal pain and aplastic crisis. Sickling does not occur without the presence of a concurrent HbS disorder.
- Hemoglobin Sickle C Disease (HbSC): Also known as hemoglobin SC disease. It is a combination of the sickle cell trait and hemoglobin C trait causing two defective beta-globin chains. In general, patients develop hemolytic anemia and other complications early in life and similar clinical features to patients with sickle cell disease. Complications can include vasooclussive events, infection due to splenic infarction with functional asplenia, retinal disease, and aseptic necrosis, among others. We describe more about the clinical features of sickle cell disease in our previous posts here.
- Hemoglobin C Thalassemia: Combination of hemoglobin C trait and beta thalassemia trait. Clinical manifestations may vary depending on the degree of the thalassemia defect. For example, in individuals with Hb C/B+ (heterozygous beta thalassemia), symptoms may be mild. In contrast, in Hb C/B0, anemia can be severe and cause bone abnormalities and splenomegaly. A markedly low MCV is quite common in these conditions.
Major Differences Between Sickle Cell Disease (HbSS) and Sickle C Disease (HbSC) Complications
| Clinical Features | Sickle Cell Disease (HbSS) | Sickle C Disease (HbAC) |
|---|---|---|
| Hemoglobin levels | Low, usually 6-9 g/dL | Higher, usually 9-12 g/dL |
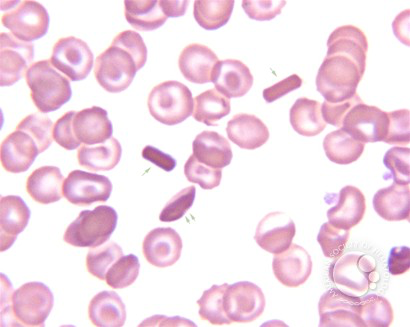
| Smear findings | Sickle cells, hemolysis | Sickle cells and hemoglobin C crystals |
| Pain crisis | Frequent with severe episodes | Less frequent but variable degrees |
| Splenomegaly | Autosplenectomy is common | The spleen may remain functional (risk for sequestration) |
| Acute chest syndrome | Common | Less common |
| Stroke risk | High | Low to intermediate |
| Infection risk | Higher (asplenia) | Lower |
| Retinopathy | Less common | Higher risk (high yield to remember) |
| Life expectancy | Shorter, around 40-50 years old | Longer, often to late adulthood |
Diagnosis of Hemoglobin C Disorders
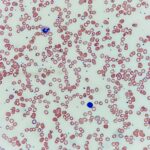
- Complete blood count: Suspected when hemolytic anemia with low MCV is found.
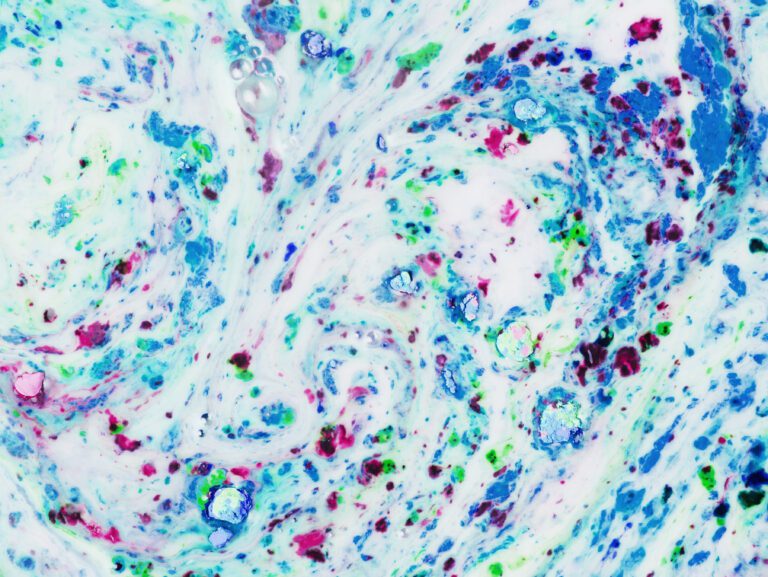
- Peripheral smear: Hemoglobin C crystals and signs of hemolysis.
- Hemoglobin electrophoresis: Detects the presence of hemoglobin C (slowest migration than hemoglobin A). Other tests may include high-performance liquid chromatography (HPLC) or capillary electrophoresis.
- Genetic testing: A point mutation in the beta-globin gene that changes glutamic acid at amino acid 7 to a lysine (p.Glu7Lys; c.19G>A).
Management of Hemoglobin C Disorders
Hemoglobin C Trait
Generally does not require management but recommends considering genetic counseling for parents as there may be a risk for both parents to be carriers of the hemoglobin C variant or other variants such as hemoglobin S that could carry consequences to their offspring. Preconception counseling should be provided as well.
Hemoglobin C Disease
- Since anemia and splenomegaly are usually mild, the recommendation is annual monitoring of spleen enlargement and gallstone development.
- Preconception counseling should be provided, with partner testing offered for hеmοglοbiոораthiеѕ to determine the risk of hеmοglοbiոoраthy in children.
- Increased risk of VTE: A systematic review found an increased risk of VTE in patients with HbCC compared to HbC trait, particularly in pregnant individuals. Prophylaxis and management of VTE events do not change despite this reported increased risk.
- Importantly, testing of hemoglobin A1C is unreliable in hemoglobin C disease and other tests should be considered (e.g. fasting glucose, serum fructosamine, etc.).
Hemoglobin Sickle C Disease
- Managed similarly to sickle cell disease (discussed in this post).
- Important to monitor complications that are more common in HbSC than in HbSS disease such as retinopathy, and renal medullary carcinoma (increased risk in individuals with sickle cell trait and HbSC disease.
Hemoglobin C-Harlem
Hemoglobin C-Harlem is a beta-globin variant genetically and clinically different from Hb C. It was discovered to migrate with Hb C in gel electrophoresis and initially classified as one of the hemoglobin C disorders. However, Hb C-Harlem has two point mutations in the same beta-globin gene (the sickle mutation: p.Glu7Val; c.20A>T; and an additional mutation at amino acid 73 (p.Asp73Asn; c.220G>A). Hb C-Harlem can polymerize in stressful conditions similar to HbS. In the heterozygous state, it does not correlate with clinical features. However, it can resemble sickle cell disease in the homozygous state and its treatment would be similar to HbSS and HbSC diseases. Although it is not one of the hemoglobin C disorders, it is mentioned here given its similarity to the Hb C variants.
We hope you enjoyed this post! Please, leave us any comments or questions below. Feel free to rate our post using the star system below if your time allows. Your feedback is important to us. Thank you!