Hemoglobin S disorders or sickle cell disease (SCD) refers to a group of disorders in which there is an abnormal beta-globin gene affecting the production of hemoglobin A (composed of 2 alpha and 2 beta-globin chains). Sickle cell disease is the most common inherited hemoglobin disorder.
Post Outline:
- Epidemiology of Sickle Cell Disease
- Genetic Abnormalities in Hemoglobin S Disorders
- Inheritance of Hemoglobin S Disorders
- Terminology in Hemoglobin S Disorders
- Classification of Hemoglobin S Disorders
- Pathophysiology of Hemoglobin S Disorders
- Clinical Manifestations and Complications of Hemoglobin S Disorders
- Diagnosis of Hemoglobin S Disorders
- Prognosis of Sickle Cell Disease
Epidemiology of Sickle Cell Disease
- Sickle cell disease (SCD) affects about 100,000 people in the United States.
- More than 90% of affected individuals are non-Hispanic Black or African American, and an estimated 3%–9% are Hispanic or Latino.
- The estimated life expectancy of those with SCD in the United States is more than 20 years shorter than the average expected (source: Centers for Disease Control CDC)
Genetic Abnormalities in Hemoglobin S Disorders
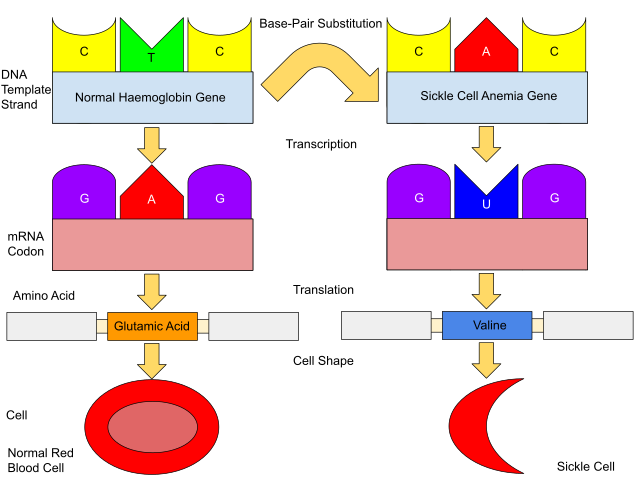
Hemoglobin S disorders occur due to a point mutation in the beta-globin gene (HBB) located on chromosome 11. The mutation causes a single base substitution of glutamic acid for valine at amino acid 7 as seen in the diagram below:
Inheritance of Hemoglobin S Disorders
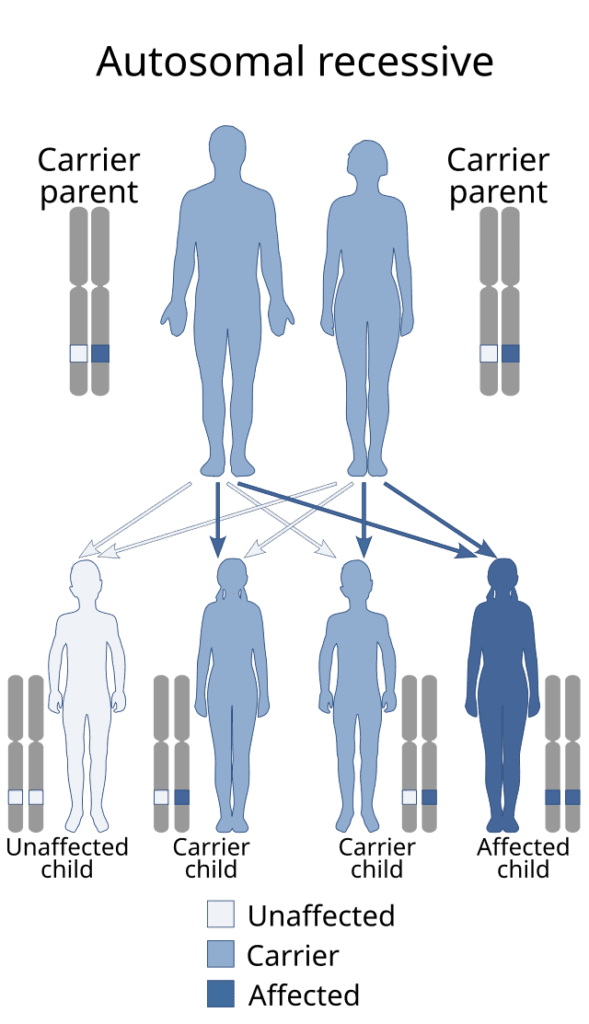
- Hemoglobin S disorders are autosomal recessive.
- Trait: One beta-globin gene affected with one normal beta gene (HbSA) causing heterozygous status.
- Hemoglobin SS disease or sickle cell anemia (SCA): Two abnormal copies of beta-globin causing homozygous status.
- Compound status: Combination with other hemoglobin disorders such as hemoglobin C (e.g. HbSC disease).
Terminology in Hemoglobin S Disorders
- Hemoglobin S trait or carrier: Affected individual with one mutated beta-globin gene (heterozygous state).
- Compound state: Presence of an abnormal globin gene with a second abnormal globin gene (alpha or beta thalassemia, hemoglobin C/D/E disease).
- Sickle cell disease (SCD): In general, used to describe conditions that cause clinical manifestations such as the compound or combined hemoglobin abnormalities (e.g. hemoglobin SC disease).
- Sickle cell anemia (SCA) or hemoglobin SS disease: Affected individual with two abnormal copies of the beta-globin gene (homozygous state). The most severe clinical form of hemoglobin S disorders.
Of note, the beta-globin gene mutation causes an inability to produce normal hemoglobin A (HbA is composed of alpha and beta-globin chains). The result is an increased production of hemoglobin S (higher HbS production is related to higher severity of the disease). The fact that hemoglobin S is elevated in SCD does not mean that the primary problem is the increased production of HbS but rather the inability to produce HbA.
Classification of Hemoglobin S Disorders
Here is a classification of the most relevant hemoglobin S disorders/sickle cell diseases (SCDs):
| Condition | Genotype/Hemoglobin Present | Disease Severity | Comments |
|---|---|---|---|
| Sickle Cell Trait | HbAS (both HbA and HbS present) | Mild/asymptomatic | Carrier status, chronic complications can occur |
| Sickle Cell Anemia (SCA) | HbSS | Severe | Severe form of SCD, many clinical implications |
| Hemoglobin SC Disease | HbSC (one HbS and one HbC present) | Moderate to severe | Milder than SCA but can be severe as well |
| Sickle B⁰ Thalassemia | HbS/β⁰ thalassemia (HbS alone) | Severe | No HbA, similar severity to SCA |
| Sickle β⁺ thalassemia | HbS/β⁺ thalassemia (HbS and a small amount of HbA) | Moderate | Less severe than SCA as there is a small amount of HbA |
| Hemoglobin SC disease | HbSD (HbS and HbD) | Moderate | Rare disorder with the presence of HbD combined with HbS |
| Hemoglobin SE disease | HbSE (HbS and HbE) | Mild | Milder form of SCD |
Pathophysiology of Hemoglobin S Disorders
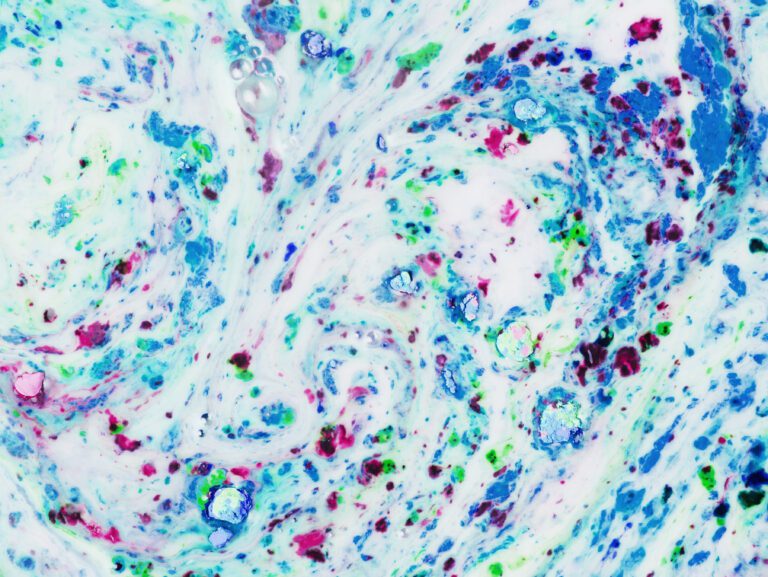
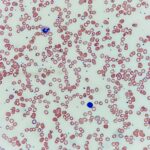
The main consequence of the beta-globin mutations in hemoglobin S disorders is the increased production of HbS with the polymerization of hemoglobin under stress (hypoxia, acidosis, dehydration, among others). The result of polymerization of HbS is the deformation of RBCs into an elongated or sickle shape leading to the obstruction of blood vessels and decreased perfusion of organs and tissues. Another important consequence is hemolysis which can occur both in the intra and extravascular spaces. Other deleterious effects include the production of pro-inflammatory substances (cytokines, chemokines, histamine, thrombin, heme) and other mechanisms that contribute to end-organ damage.
Vaso-Occlusive Events (VOEs)
Vaso-occlusion is common in hemoglobin S disorders as they cause tissue ischemia and infarction. Although vaso-occlusion is a constant process in SCD/SCA, acute events can occur and carry significant morbidity and mortality. In general, VOEs refer to those acute events that lead to medical care or consequences including:
- Acute vaso-occlusive events: Episodes of worsening ischemia causing intense pain in several areas and other symptoms such as nausea, vomiting, fatigue, and others. Bone infarction and dactilitis is common.
- Acute chest syndrome (ACS): Acute ischemia located in the chest tissue is generally complicated with thrombotic and infectious events. Fever, chest pain, and shortness of breath are the most common symptoms (the clinical picture is similar to pneumonia).
- Renal infarcts.
- Cardiovascular events include acute myocardial infarction, stroke, venous thromboembolism, and priapism, among others.
Clinical Manifestations and Complications of Hemoglobin S Disorders
The clinical manifestations in hemoglobin S disorders depend on the type and severity of the affected beta-globin gene mutation.
Sickle Cell Trait
Patients with sickle cell trait are generally asymptomatic and do not develop vaso-oclussive and other acute complications. However, these patients are at increased risk of the following complications:
- Exertional rhabdomyolysis: Rare complications that can occur with strenuous physical activity. It can be one of the factors associated with sudden death in this population.
- Venous thromboembolism: Deep vein thrombosis and pulmonary embolism.
- Kidney disease: Hyposthenuria (abnormally low urine sediment content or “dilute urine”), which can lead to dehydration. There is an increased risk for chronic kidney disease (CKD) and end-stage kidney disease (ESKD), proteinuria, hematuria, and renal medullary carcinoma (extremely rare).
- Cardiovascular diseases: Hypertension, diabetes, stroke, and myocardial infarction.
- Other vaso-occlusive complications: Splenic infarcts at high altitudes, and retinopathy.
Sickle Cell Disease/Sickle Cell Anemia
Clinical manifestations of SCD/SCA can be classified into acute and chronic:
Acute Clinical Manifestations
- Infection: Mostly related to encapsulated organisms (especially Streptococcus pneumoniae and Haemophilus influenza). Patients should receive pneumococcal, Hib, meningococcal, and influenza vaccines.
- Profound anemia: This could be related to aplastic crisis and hyperhemolysis. Hyperhemolysis occurs usually during an acute VOE in which the body cannot compensate for the degree of hemolysis.
- Splenic sequestration: Presents as hypovolemic shock and could be fatal. It is characterized by an acute drop in hemoglobin level, typically 2 g/dL below baseline.
- Acute VOEs.
- Acute chest syndrome.
- Kidney infarction.
- Dactilitis and bone infarcts.
- Cardiovascular conditions such as stroke and myocardial infarction.
- Priapism.
Chronic Clinical Manifestations
- Pain: Other than VOE, patients can experience severe chronic pain and likely have a baseline level of pain that cannot be completely eradicated.
- Chronic anemia.
- Iron overload: related to SCD and blood transfusions.
- Neurologic disorders and seizures.
- Pulmonary hypertension.
- Hypertension and increased cardiovascular disease.
- Osteoporosis and osteopenia.
- Congestive heart failure.
- Chronic liver disease and pigment-related cholelithiasis.
- Delayed growth and puberty.
- Chronic leg ulcers.
- Eye disorders include proliferative retinopathy and others.
- Psychological stress, social inequities, and inequality in medical care.
Many other complications could be seen in individuals with SCD/SCA. Therefore, the management of these patients requires a multidisciplinary team.
Diagnosis of Hemoglobin S Disorders
- Most patients are diagnosed with the identification of hemoglobin S.
- In the United States, the majority of states perform a screening for sickle cell disease on all newborns.
- Patients should be tested when suspected and when found to have evidence of anemia, hemolysis, and a family history of anemia. Usually, the initial test to perform is a hemoglobin electrophoresis to measure the different types of hemoglobin (e.g. In SCA, a high level of HbS would be found).
- Laboratory techniques for diagnosis: high-performance liquid chromatography (HPLC), isoelectric focusing (IEF), or gel electrophoresis techniques. For children and adults, the combination of HPLC and IEF allows for a definitive diagnosis of a sickle cell disorder.
- Polymerase chain reaction (PCR) or DNA sequencing may also be used.
- Diagnostic confirmation – For children and adults, the combination of HP
Prognosis of Sickle Cell Disease
- Survival of individuals with SCD is reduced compared with those without SCD, but the prognosis for SCD has been steadily improving in the last decade.
- Comprehensive care leading to improved outcomes includes newborn screening, immunizations, antibiotic prophylaxis, medications (such as hydroxyurea, voxelotor, and crizanlizumab, among others), and prevention and treatment of disease complications.
- In the United States, the median survival of adults with Hb SS and Hb S-beta0 is 58 years, and the median survival for Hb SC and Hb S-beta+ was 66 years.
- Many new treatment options are being developed and hopefully will continue to improve the quality of life and outcomes of patients with hemoglobin S disorders.
In the next post, we will discuss the management of sickle cell disease focusing on the treatment of sickle cell anemia. We hope you enjoyed this post! Please, leave us any comments or questions below. Rate our post using the star system below if your time allows.
Thank you for reading!