Vitamin B12 or cyanocobalamine deficiency is found frequently in the medical practice. B12 deficiency is the most common cause of macrocytic anemia and can occur in individuals of any age. This post will describe an overview of the key features to consider when assessing and managing a patient at risk or who has developed vitamin B12 deficiency.
Table of contents:
- Epidemiology of Vitamin B12 deficiency:
- Pathophysiology of Vitamin B12 Deficiency
- Causes of Vitamin B12 Deficiency
- Dietary Sources of Vitamin B12
- Clinical Manifestations of Vitamin B12 Deficiency
- The Role of Methylmalonic Acid in Nerve Damage
- Diagnosis of Vitamin B12 Deficiency
- Management of Vitamin B12 Deficiency
Epidemiology of Vitamin B12 deficiency:
- Vitamin B12 deficiency constitutes 1-2% of all causes of anemia.
- B12 deficiency can occur at any age but is more frequent in the elderly population.
- Pernicious anemia (autoimmune gastritis) is more commonly observed in individuals of Northern European descent (incidence is 1-2% of adults versus 0.1% in the general population).
Pathophysiology of Vitamin B12 Deficiency
- Vitamin B12 is sensitive to acid in the stomach and gut environment. Therefore, it needs to be protected until it is absorbed.
- Two ” chaperones ” bind to B12 and protect it, allowing it to reach its final destination: the distal gut (ileum) where it gets absorbed.
- When ingested, vitamin B12 binds to a protein present in the saliva called R-factor (the first chaperone). When the B12/R-factor complex arrives in the small intestine, B12 is cleaved from the R-factor by pancreatic enzymes, allowing it to bind to its second chaperone, the one and only intrinsic factor (IF).
- Intrinsic factor is secreted by the parietal cells of the stomach. When bound, the B12/IF complex allows B12 to be transported through the small intestine until it reaches the last portion where it gets absorbed, the ileum.
- The ileum has receptors that only bind the B12/IF complexes. Therefore, without intrinsic factor, B12 is not absorbed. This explains the pathophysiology of pernicious anemia in which there is decreased production of IF due to the destruction of parietal cells in the stomach.
It is key to recognize that vitamin B12 needs two chaperones. My way of remembering B12 absorption is to think that B12 needs chaperones. Therefore, it must be traveling far away (absorption in terminal ileum). In contrast, iron absorption occurs in the proximal intestine (duodenum and jejunum). After all, iron is made of “metal” and does not need those chaperones.
Causes of Vitamin B12 Deficiency
- Malabsorption: Any abnormality in the absorption process mentioned above could cause B12 deficiency. For example, a gastric bypass could decrease the availability of IF and lead to B12 deficiency.
- Anatomic abnormalities: Gastric bypass, bowel resection.
- Inflammatory diseases affecting the intestine: celiac disease or inflammatory bowel disease (Chron’s disease).
- Intestinal infections such as bacterial overgrowth, tapeworms Diphyllobothrium latum.
- Autoimmune: Pernicious anemia is the classic example. Autoantibodies against intrinsic factor or parietal cells affect the production of IF leading to B12 deficiency.
- Dietary insufficiency: Animal sources of B12 such as strict vegan diet for approximately 3 years.
- Pancreatic insufficiency: Inability to cleave R-protein.
- Medications: Some drugs can impair or block the absorption of B12 including proton pump inhibitors, histamine 2 receptor antagonists, metformin, neomycin, and nitrous oxide (anesthesia or recreational use).
Dietary Sources of Vitamin B12

- Vitamin B12 is found mostly in animal proteins such as meat, fish, eggs, and dairy.
- Many foods are fortified with B12 including plant-based milk, cereal, nutritional yeast, and others.
- Supplements are available and recommended for individuals with strict vegan diets to avoid deficiency.
Clinical Manifestations of Vitamin B12 Deficiency
- Classic symptoms of anemia: fatigue, lightheadedness, palpitations, shortness of breath, paleness.
- Macrocytic or megaloblastic anemia: cells grow and get larger but cannot divide due to impaired DNA synthesis.
- Glossitis.
- Diarrhea.
- Headaches.
- Neuropsychiatric disorders: Mood changes, sleep difficulties, among others.
- Nerve injury: Diverse neurologic symptoms can occur. Nerves from the posterior columns could get damaged and can lead to subacute combined degeneration of the spinal cord (SCDSC). Nerves in the posterior columns are motor and sensory (hence the term “combined motor and sensory deficits”). SCDSC presents as ataxia, loss of proprioception, dementia, and peripheral neuropathy. The cause of nerve involvement in B12 deficiency is the elevation of methylmalonic acid (MMA).
- Others: Other symptoms can be present depending on the etiology of B12 deficiency. For example, bloody diarrhea could occur in Chron’s disease.
The Role of Methylmalonic Acid in Nerve Damage
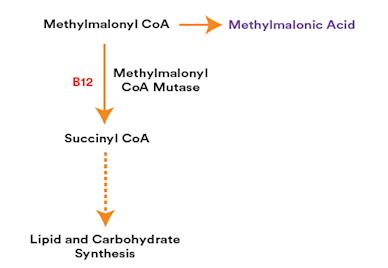
Vitamin B12 is needed by the enzyme methyl malonyl coenzyme A mutase to transform MMA into succinyl coenzyme A. As seen in the graph above, if B12 is deficient, the process cannot occur properly leading to MMA excess. MMA could affect myelin synthesis by interfering with its fatty acid metabolism. MMA also generates reactive oxygen species and can lead to impaired mitochondrial function.
Diagnosis of Vitamin B12 Deficiency
- Complete blood count (CBC): Assess for macrocytic anemia (MCV >100 fL). B12 deficiency can also lead to pancytopenia.
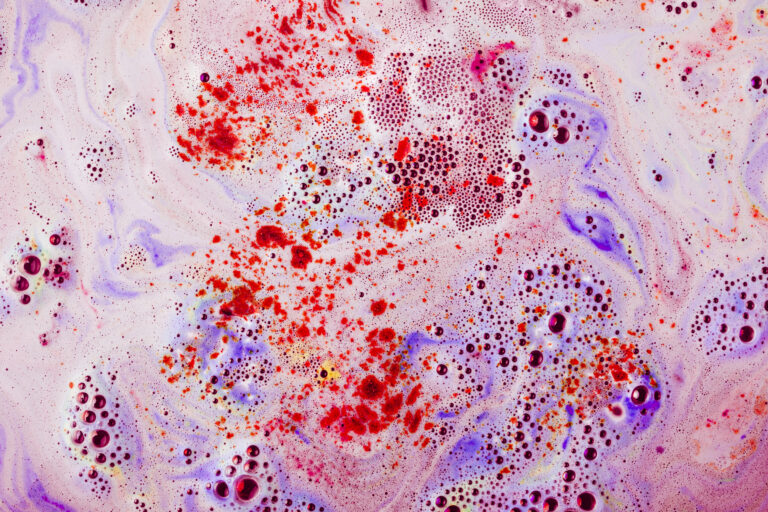
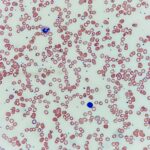
- Peripheral blood smear:
- Differences in the size (anisocytosis) and shape (poikylocytosis) of red blood cells (RBCs) could be found due to the larger cells caused by B12 deficiency.
- Ovalocytes are commonly found due to the larger RBCs losing their conventional biconcave shape.
- Hypersegmented neutrophils: There are two main criteria for hypersegmentation. First, having at least one neutrophil with 6 or more lobes in the nucleus. Second, 5% or more of neutrophils have 5 or more lobes.
- Pancytopenia and some dysmorphic features could also be seen in severe cases.
- Hemolysis can occur in B12 deficiency due to increased rigidity of RBCs and abnormalities in their cell membrane: check LDH (elevated), haptoglobin (decreased), indirect bilirubin (increased), and reticulocyte index (increased although can be normal or decreased when the nutritional deficiency is severe)
- Vitamin B12 levels: Importantly, serum B12 levels have poor sensitivity and specificity (highly variable binding to B12 binding proteins transcobalamine and haptocorrin). A serum B12 above 300 pg/mL is “normal.” B12 levels between 200 and 300 pg/mL are considered “borderline,” and further enzymatic testing may be helpful in diagnosis. Patients with B12 levels below 200 pg/mL are considered “deficient.”
- Enzymatic testing: Methylmalonic acid and homocysteine are sensitive to diagnose B12 deficiency (>90%). However, MMA is more sensitive and specific and is the recommended test to perform for all patients with clinical features of B12 deficiency, or those who are asymptomatic but are found to have borderline levels of B12. Homocysteine levels are generally not recommended as many disorders can elevate homocysteine such as folate and pyridoxine deficiency and hypothyroidism.
- Functional tests: There are no validated B12 functional tests. Historically, the Schilling test was used to assess B12 absorption by administering a radioactive B12 and measuring its excretion in the urine. Other tests such as the Cobasorb have not been validated.
- Others: Intrinsic factor antibodies and parietal cell antibodies can be considered when pernicious anemia is suspected. Other tests including investigation of malabsorption and referral to specialists such as gastroenterology should be considered as well.
A key consideration is that the diagnosis of vitamin B12 deficiency should be suspected clinically and supported by laboratory testing. When the suspicion of vitamin B12 deficiency is high, the recommendation is to check both the vitamin B12 level and MMA. If MMA is elevated, it supports the diagnosis of vitamin B12 deficiency even in the setting of normal B12 levels.
Management of Vitamin B12 Deficiency
Treatment of vitamin B12 deficiency is aimed towards repletion of vitamin B12. The two main ways of administering B12 are oral and intramuscular. Here are a few general considerations to consider for the management of B12 deficiency:
- Who needs rapid correction?: Individuals with symptomatic anemia, neuropsychiatric symptoms, neurological symptoms, SCDSC, or when used as initial loading therapy before switching to long-term oral B12.
- Parenteral treatment (intramuscular or subcutaneous) can be considered in those who need rapid correction.
- Oral treatment is adequate for most patients except those with considerable malabsorption or anatomic abnormalities of the distal gut.
- High-dose oral B12 is absorbed passively (1-4%) even with decreased levels of IF. Therefore, oral B12 can still be considered an option for patients with pernicious anemia. Adherence to oral B12 could be a barrier to being carefully monitored.
- Duration of treatment depends on whether the cause of B12 deficiency is reversible. For example, if an infection is a likely cause, treatment should be considered until the infection has resolved. If the cause is not reversible, B12 should be used indefinitely.
- It is crucial to treat the underlying cause of B12 deficiency.
- B12 is safe and well tolerated even at high doses.
- Assess for concomitant folate deficiency.
Vitamin B12 Dosing
- Oral vitamin B12: Cyanocobalamine 1,000 to 2,000 mcg daily (choose the higher dose in patients with pernicious anemia or malabsorptive symptoms (unless severe).
- Intramuscular or subcutaneous (IM or SC): Cyanocobalamine 1,000 mcg IM or SC per administration. If rapid correction is desired, it can be administered as 1,000 mcg once daily or every three days in the first week, then 1,000 mcg weekly for 4 weeks, followed by 1,000 mcg monthly.
Monitoring Response to B12 Administration
- Initial response includes reticulocytosis within 3-5 days, increased hemoglobin over 1-2 weeks, and resolution of anemia and other cytopenias in 4-8 weeks.
- If not severe, consider repeat testing including CBC and hemolysis markers, B12 levels, and MMA 8-12 weeks after starting B12 administration.
- In more severe cases, consider repeat testing in 4-8 weeks and adjust treatment as appropriate. If inadequate response to oral B12, switch to IM or SC.
- Resolution of neurological complications can take longer and some symptoms may not fully recover depending on the duration and severity of the neurological injury.
- Monitor for hypokalemia during the initial week of treatment. There is increased potassium uptake during the production of new blood cells that could lead to depletion. However, this is a rare complication that does not cause clinical consequences in the majority of patients.
We hope you enjoyed this post! Please, leave us any comments or questions below. Feel free to rate our post using the star system below if your time allows. Your feedback is important to us. Thank you!