The most common cause of anemia in the United States and worldwide is iron deficiency anemia (IDA). IDA affects more than 12% of the world’s population, particularly women, children, and individuals living in developing countries. There are many opportunities to impact the lives of people with iron deficiency. This post will describe the most relevant points to consider in this condition and an approach to its diagnosis and management in adults.
Causes of Iron Deficiency
There are many causes of iron deficiency. However, in the United States, bleeding is the most common cause while insufficient dietary intake is the leading cause worldwide. We can divide the causes of iron deficiency into two categories:
- Decreased intake or absorption:
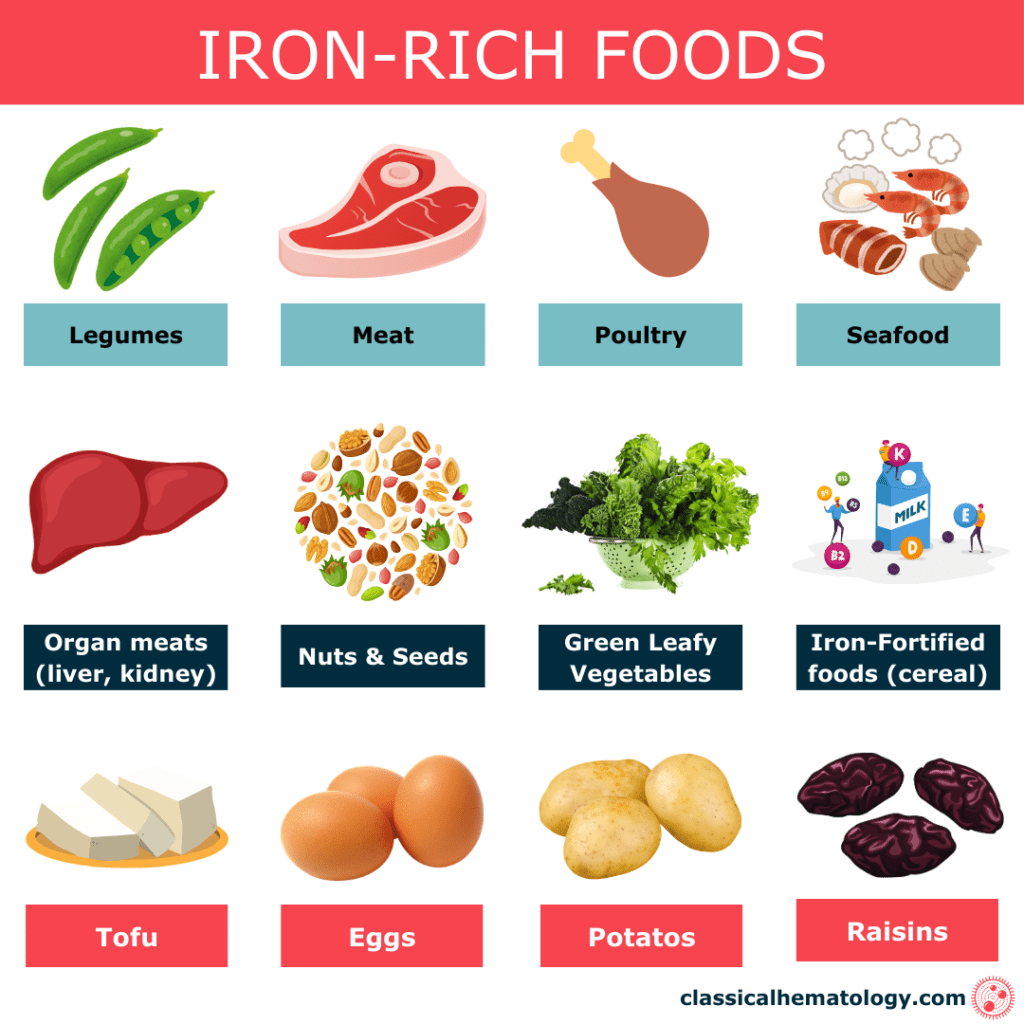
- Decreased intake: This can be seen in vegetarians, vegans, and other diets with insufficient iron content. Lack of availability of iron-rich foods and fortification of products is the main reason for dietary deficiency in developing countries.
- Decreased absorption: Associated with malabsorptive syndromes such as celiac disease, H. Pylori infection, gastritis, bariatric surgery, use of antiacid medications, etc.)
- Iron loss: Bleeding is the most common cause and can be gastrointestinal, genitourinary, menstrual (frequently underestimated), and any other source of bleeding. Iron loss can also be seen in pregnancy, lactation, gastrointestinal parasites, frequent blood donation or blood draws, and others.
There are other rare causes of iron deficiency such as:
- Erythropoiesis-stimulating agents (ESAs): These medications can cause iron deficiency mainly due to the increased need for iron when producing RBCs, and redistribution of iron into newly formed RBCs.
- Urinary and pulmonary hemosiderosis: Rare conditions in which repeated bleeding into the lungs or kidneys occurs leading to accumulation of iron in these tissues.
- Inherited disorders: Rare and caused by mutations in genes participating in iron metabolism.
Inherited Iron Deficiency Disorders
| Disorder | Genetic Basis and Consequences | Symptoms | Diagnosis | Treatment |
|---|---|---|---|---|
| Iron-refractory Iron Deficiency Anemia (IRIDA) | Mutations in the TMPRSS6 gene reduce hepcidin suppression, leading to persistently low iron absorption and utilization | Severe, persistent iron deficiency anemia unresponsive to oral iron | Low serum iron, normal to high ferritin, genetic testing | Intravenous iron |
| Atransferrinemia | Mutations in the transferrin TF gene impair iron transport by lacking transferrin, leading to deficient iron delivery to cells | Severe anemia, growth retardation, recurrent infections | Low transferrin, high serum iron, genetic testing | Plasma transfusions, iron chelation therapy |
| DMT1 Deficiency (Divalent Metal Transporter 1) | Mutations in the SLC11A2 gene cause defective iron absorption (DMT1 deficiency) from the intestine and impaired cellular iron uptake | Microcytic anemia, growth retardation | Low serum iron, high ferritin, genetic testing | Oral or intravenous iron supplements |
Iron-Rich Foods
Clinical Manifestations of Iron Deficiency
The clinical manifestations of iron deficiency anemia can be similar to other causes of anemia due to low hemoglobin levels.
Most Common Manifestations in Iron Deficiency Anemia
- Fatigue: Seen in approximately 70-90% of patients with IDA.
- Pallor: Up to 80% of patients.
- Shortness of breath: Up to 70% of patients.
- Dizziness: Up to 60% of patients.
- Headaches: Up to 50% of patients.
Other Less Common Manifestations of Iron Deficiency Anemia
- Pica (10-30%): Desire or compulsion to eat substances that do not qualify as foods such as ice, dirt, clay, and paper, among others.
- Restless leg syndrome (Willis-Ekbom disease) (10-25%): an uncomfortable urge to move the legs during periods of inactivity.
- Nail deformities (20-40%): Brittle or spoon-shaped nails (koilonychia).
- Glossitis (5-15%): Inflammed or shiny tongue.
- Plummer-Vinson syndrome: esophageal webs causing dysphagia (rare).


Diagnosis of Iron Deficiency Anemia
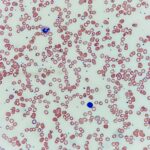
When there is a clinical suspicion of iron deficiency anemia, readily available blood tests can be performed including a complete blood count (CBC) and chemistries including an iron panel. Importantly, most iron deficiency anemias will have a low hemoglobin with microcytosis (mean corpuscular volume MCV <80) and reactive thrombocytosis could also be present (mostly due to increased bone marrow hematopoiesis stimulated by several substances such as erythropoietin).
Here is a summary of the iron panel tests available:
| Test | Description | When to Test | Low (↓) | High (↑) |
|---|---|---|---|---|
| Iron | Measures the amount of iron in the blood | Suspected iron deficiency/ anemia, anemia of inflammation | Iron deficiency/ anemia, bleeding, malnutrition, malabsorption | Hemochromatosis, liver disease |
| Total Iron Binding Capacity (TIBC) | Measures the total amount of iron that can be bound by transferrin proteins in the blood | Suspected iron deficiency/ anemia, anemia of inflammation | Iron overload disorders, pregnancy | Iron deficiency anemia, chronic disease, malnutrition (think of TIBC truly missing his iron friend) |
| Transferrin Saturation (Tsat) | Calculates the percentage of transferrin saturated with iron | Suspected iron deficiency/ anemia, anemia of inflammation | Iron deficiency anemia, chronic disease, malnutrition | Iron overload disorders, liver disease |
| Ferritin | Reflects iron storage in the body (also an acute phase reactant) | Suspected iron deficiency/ anemia, anemia of inflammation, inflammatory marker | Iron deficiency/ anemia, chronic disease, malnutrition | Inflammation, infection, hemochromatosis, iron overload disorders, inflammation |
Laboratory Evidence of Iron Deficiency
Ferritin is a reliable test to assess total iron storage in the body. However, it is important to remember that inflammatory and other chronic conditions can lead to increased ferritin levels and possibly mask iron deficiency. Therefore, obtaining a full iron panel with other tests such as TIBC, transferrin saturation, and iron level is recommended to get a better picture of iron disorders. When ferritin is <30 ng/mL, the diagnosis of iron deficiency anemia is confirmed. However, testing could be inconclusive sometimes and it requires the interpretation of the entire iron panel. Here is a summary of the possible scenarios you may encounter in clinical practice:
Here’s a table outlining common clinical scenarios seen in practice where iron deficiency might present with discrepant findings, such as high ferritin but low transferrin saturation (TSAT), and how to differentiate these conditions:
Clinical Scenarios with Discrepant Findings in Iron Studies
| Scenario | Lab Findings | Associated Conditions | How to Differentiate |
|---|---|---|---|
| High Ferritin, Low TSAT | High ferritin (>100 ng/mL), low TSAT (<20%) | Chronic Inflammation or Infection: Ferritin is an acute-phase reactant that increases with inflammation, masking iron deficiency. Chronic Kidney Disease (CKD): Reduced erythropoietin leads to functional iron deficiency, despite high ferritin | –C-Reactive Protein (CRP)/Erythrocyte Sedimentation Rate (ESR): Elevated levels indicate inflammation. -Kidney Function Tests: May show chronic kidney disease |
| Low Ferritin, Normal TSAT | Low ferritin (<30 ng/mL), normal TSAT (20-50%) | Early Iron Deficiency: Ferritin is depleted before serum iron and TSAT decrease | Treat iron deficiency and monitor levels |
| Normal Ferritin, Low TSAT | Normal ferritin (30-100 ng/mL), low TSAT (<20%) | Functional Iron Deficiency: Iron is sequestered in reticuloendothelial system, not available for erythropoiesis. Early Stages of Iron Deficiency: Body uses up serum iron while storage remains normal. | Can measure Soluble Transferrin Receptor (sTfR): Elevated in iron deficiency |
| Low Ferritin, Low TSAT, Normal Hemoglobin | Low ferritin (<30 ng/mL), low TSAT (<20%), normal Hb | Subclinical Iron Deficiency: Iron depletion without anemia. Iron Deficiency in Early Stages: Not yet affecting hemoglobin. | Treat iron deficiency even if no anemia is present |
| Low Ferritin, Low TSAT, Low Hemoglobin | Low ferritin (<30 ng/mL), low TSAT (<20%), low Hb (<12 g/dL) | Iron Deficiency Anemia (IDA): Classic presentation of iron deficiency. | -Assess for bleeding, decreased intake or absorption of iron -Treatment of iron deficiency |
As you can note in the table, both ferritin and Tsat decrease with iron deficiency while TIBC usually increases. Ferritin and Tsat are the two most helpful tests to evaluate iron deficiency. The soluble transferrin receptor (sTfR) is rarely used in clinical practice but can be considered for those cases in which there is uncertainty about the diagnosis.
Treatment of Iron Deficiency

One of the most important aspects of the treatment of iron deficiency is to identify the cause. The main causes to look for in the United States would be bleeding and malabsorption syndromes. If the cause is not obvious, additional evaluations may include gastroenterology referral for endoscopy and testing for conditions that decrease absorption, especially in individuals age 50 or older and those who do not have a response to iron repletion (testing for H. Pylori, celiac disease, atrophic gastritis, etc.).
Treatment of Iron Deficiency Without Anemia
Iron deficiency can cause symptoms and affect the quality of life of individuals. Therefore, it is recommended to treat all patients with iron deficiency regardless of the presence of anemia. Importantly, a healthy diet provides enough iron in normal conditions but is insufficient for the treatment of established iron deficiency. In general, treatment of iron deficiency without anemia can be done with oral iron unless there is clinical suspicion of malabsorption or if patients cannot tolerate oral iron due to side effects including abdominal pain, constipation, and others.
Treatment of Iron Deficiency Anemia
A recommended approach to the treatment of iron deficiency anemia is to differentiate between complicated and uncomplicated iron deficiency. Here is a figure with recommendations for the management of iron deficiency anemia:
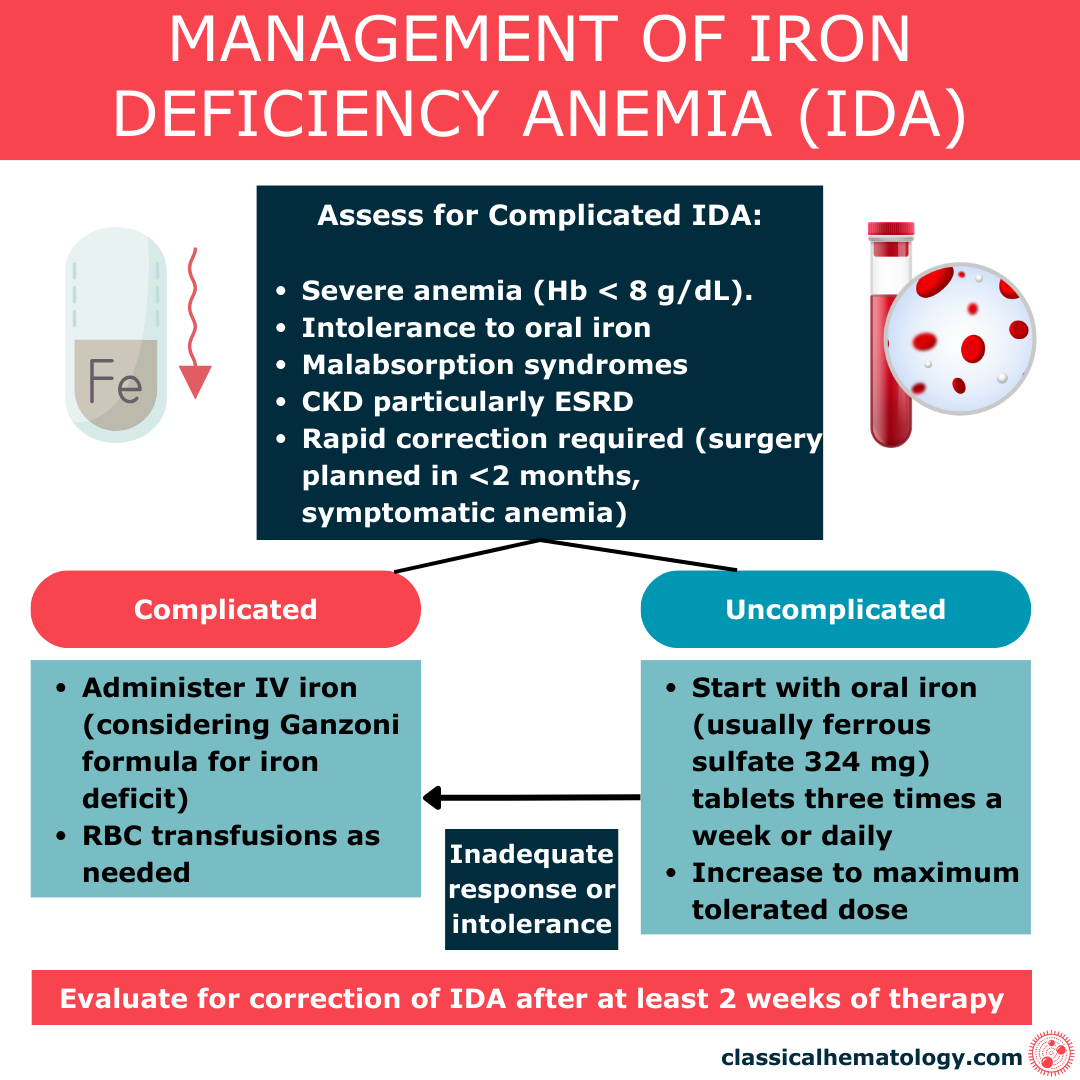
The IV formulation to be used depends on several factors but it is important to familiarize yourself with the products available in your institution. IV iron administration is safe and the risk of side effects has decreased with the newer products that are available. Here is a list of adverse events that can be seen with IV iron administration:
Adverse Effects of IV Iron Administration
Common Adverse Events
- Nausea
- Injection Site Reactions: Including pain, swelling, or bruising at the injection site
- Flushing
- Headaches
- Dizziness
- Hypotension: Usually mild and transient
- Fever
- Fatigue
Less Common Adverse Events
- Chest pain or dyspnea
- Muscle and joint pains
- Rash or itching
- Cardiac arrhythmias (rare)
- Infection (rare, avoid IV iron in patients with sepsis)
- Hypersensitivity reactions
- Anaphylactic Reactions (rare)
Monitoring Response to Iron Administration
After the administration of iron, a modest reticulocytosis is usually seen in 7 to 10 days. However, normalization of hemoglobin takes at least six to eight weeks. Normalizing iron storage with oral iron can take up to 12 months and it is faster with IV administration. Therefore, it is important to monitor patients and assess for response or continued iron loss that could require additional administration of iron.
Evaluation
We hope you enjoyed this post! Please, leave us any comments or questions below. Rate our post using the star system below if your time allows. Thank you for reading!